Given this glimpse into the brain, one can conclude that symptoms of psychosis, including some types of dementia and schizophrenia, are mainly related to deficits in the prefrontal cortex (PFC). Hypofrontality, which is a state of decreased cerebral blood flow, causes impaired executive functioning of the prefrontal cortex (Meyer, 2019) and is present in individuals afflicted with severe mental illnesses such as schizophrenia, bipolar disorder, and major depressive disorder (MDD). The PFC is responsible for decision making, planning, personality expression, motor control, working memory, inhibition of inappropriate behaviors, and attention (Meyer, 2019).
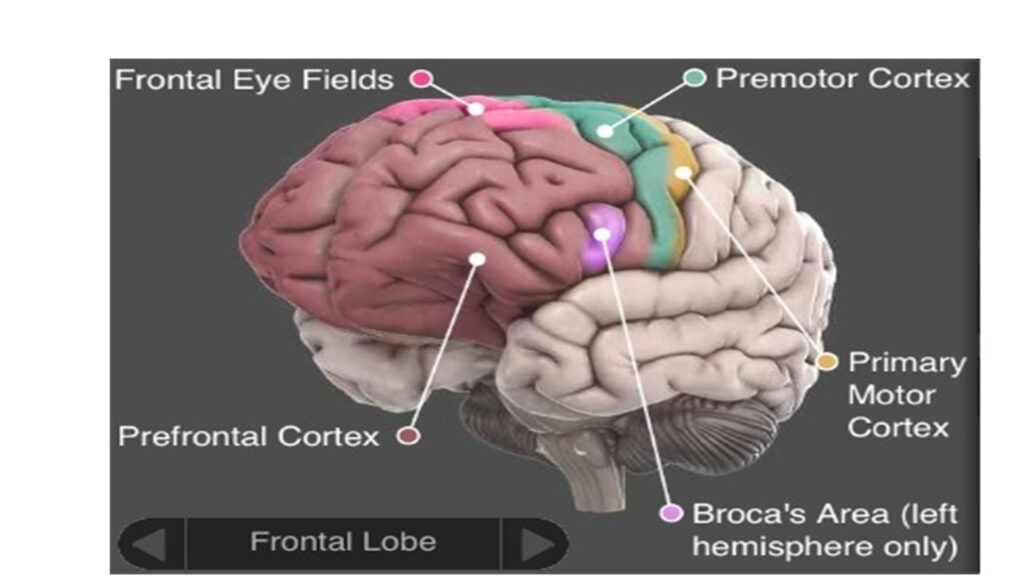 Cognitive deficits commonly seen in patients suffering from psychosis affect working memory, language and executive function, episodic memory, speed processing, attention inhibition, and sensory processing (Brisch, 2014). With damage to the PFC, there are deficits in working memory, social and cognitive impairments, poverty of speech, flat affect, and a lack of motivation (Meyer, 2019). These resemble the negative symptoms seen in individuals with schizophrenia, for example. Thus, in individuals with severe mental disorders that include psychosis we see that the PFC is unable to execute top-down control over subcortical systems resulting in the social and emotional deficits.
Cognitive deficits commonly seen in patients suffering from psychosis affect working memory, language and executive function, episodic memory, speed processing, attention inhibition, and sensory processing (Brisch, 2014). With damage to the PFC, there are deficits in working memory, social and cognitive impairments, poverty of speech, flat affect, and a lack of motivation (Meyer, 2019). These resemble the negative symptoms seen in individuals with schizophrenia, for example. Thus, in individuals with severe mental disorders that include psychosis we see that the PFC is unable to execute top-down control over subcortical systems resulting in the social and emotional deficits.
Working memory discrepancies of patients suffering from psychosis has been extensively studied by neuroscientists by examining the PFC and cognitive function. However, there are additional challenges among patients afflicted with psychosis. Auditory processing involving memory procedures is impaired as well in working memory (Brisch, 2014). In a clinical test setting, patients demonstrated significant limited capacity of their working memory, as shown by an increased rate of false positives and errors (Nenadic, 2015).